Occipital Nerve Stimulation for Cluster – Why does it “sometimes” work?
When we first discussed occipital nerve stimulation back in 2007, the results were promising, but not consistent. Now that’s not unusual for an early study. But when it comes to conditions like cluster headache, there’s another problem.
Cluster headache is certainly a rarer type of headache disorder. So when you have fewer people experiencing it, you’ll also have fewer trying a specific treatment, and fewer people in clinical trials. So it takes a long time to get results – and those results may be less reliable than they would be with a larger group.
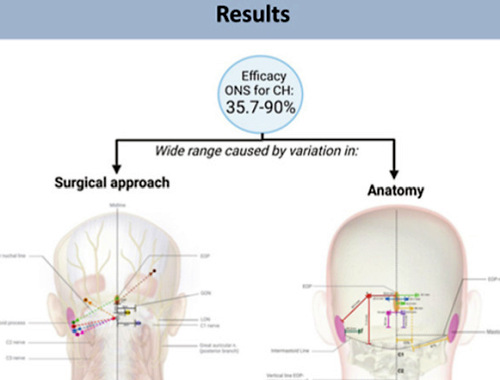
Occipital nerve stimulation remains a promising treatment today, and also a treatment that doesn’t work consistently. That fact was brought to the attention of researchers in the Netherlands, who published a study last year entitled “The Untold Story of Occipital Nerve Stimulation in Patients With Cluster Headache: Surgical Technique in Relation to Clinical Efficacy”. In their report, they included the above statistic for “efficacy” (usefulness – success) of the treatment – 35.7% to 90%! Quite a variation.
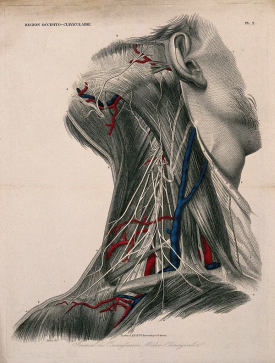
Occipital nerve stimulation involves implanting a small device surgically. The device provides “neurostimulation” for the occipital nerves. As this report points out, “the physician aims to target all the occipital nerve branches simultaneously”. The stimulation seems to interrupt pain signals, providing pain relief.
So why doesn’t it consistently “work as advertised”? The researchers found two variables. The first one is – you! The exact makeup of your body is not the same as someone else’s. You can’t just cut someone open and find the exact same nerves in the exact same place.
Now, of course, your surgeon is aware of this. But there’s only so much that a doctor can do.
One thing they can do it standardize surgical techniques. If all doctors, for example, measured in the same way when they implanted the device, we would at least have a more similar treatment.
But that’s not what’s happening. Doctors may use significantly different methods, and also record different information. That means that we can’t even properly compare clinical trials, because we can’t compare exactly what the doctor did.
These researchers are recommending certain points of standardization so that we can properly compare results. This may mean that doctors try to find the best technique based on the current research, and go with that. But it also may mean different techniques that are measured and reported in a standardized way, so that results can be better compared.
When looking for a surgeon, it would be helpful to know what the success rate of this treatment is for their patients. But it also would be nice to know what standards they are following.
This is not just a concern in cluster headache surgery, but in many types of treatment. Though we wouldn’t want to restrict doctors from the treatment they feel is best for you, we also want to make the most of each treatment, so that everyone can improve.