Do you really have “Migraine”?
So your doctor said you get “migraines”, did he? Could it really be that simple? What if I told you that “migraine” isn’t a valid diagnosis at all?
I think I can hear the mail carrier coming now – with bags and bags of hate mail. Well, hear me out before you pull out the quill and parchment to complain.
If you’ve been following my articles for a while, you’ve probably heard me say that you need to get a specific diagnosis. When a doctor says you have “headaches” or even “migraines”, that’s really pretty vague. In fact, it’s so vague, it’s almost impossible to define.
The gold standard for headache diagnosis is The International Classification of Headache Disorders, from the International Headache Society. If you go into the latest (beta) version to find out what “migraine” is, you could be in trouble.
As far as a diagnosis goes, there’s no such thing.
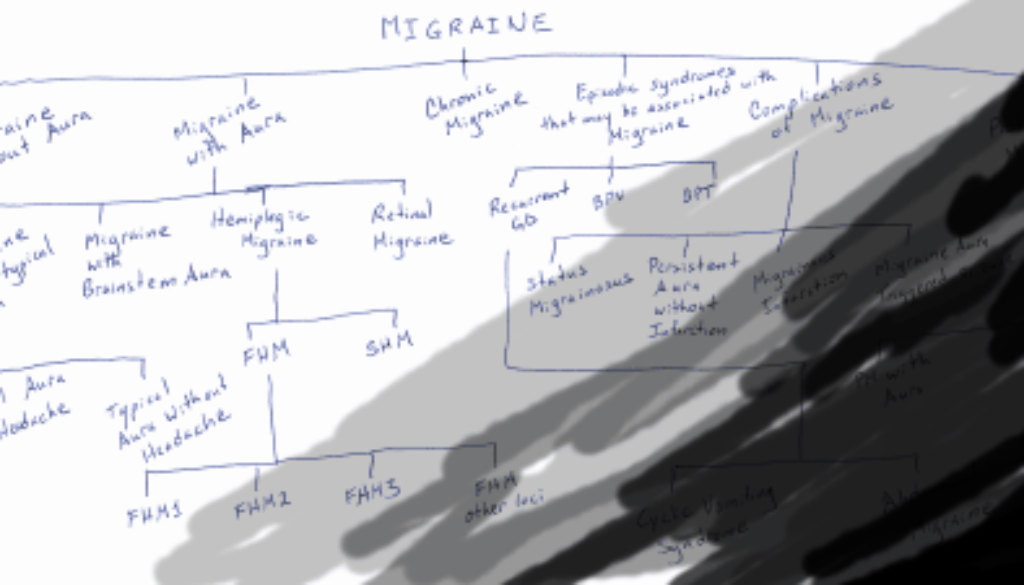
Oh yes, they do have a category called “migraine”, but there is no list of symptoms, no explanation. It’s a general category, one of four types of “primary headaches” (yes, don’t worry, they recognize that migraine does not always include headache – it’s just the technical name of the category).
The only information you’ll get about migraine is this:
Migraine is a common disabling primary headache disorder. Epidemiological studies have documented its high prevalence and high socio-economic and personal impacts. In the Global Burden of Disease Survey 2010, it was ranked as the third most prevalent disorder and seventh-highest specific cause of disability worldwide.
Ok, but what is it? Well, it’s just an umbrella category.
There are two possible types of migraine you might have – migraine without aura or migraine with aura. If you could get away with calling anything just “migraine”, it would probably be the first, although that would be confusing because so many people associate visual aura with migraine (a possible symptom in migraine with aura).
What’s the difference between the two? Well, first you need to have more attacks before you will be diagnosed with migraine without aura (5 instead of 2). Obviously aura symptoms are present in migraine with aura. And migraine without aura must include headache, and possibly nausea and sensitivity to light or sound.
Already these differences are important. When aura is present, there are certain things your doctor should rule out, such as transient ischemic attack (TIA). Frequency of the attacks could change the diagnosis, and the symptoms may be different depending on your age.
But once we get into migraine with aura, we can still get more specific. There are four sub-types of migraine with aura, with another eight possibilities under that.
And although we’ve talked about two main subtypes of migraine, you may also have chronic migraine (this is where frequency becomes important, but there may be a number of other differences), complications of migraine (maybe your attacks don’t stop, or there are seizures involved), probable migraine (a little more investigation may need to be done here, to make sure you’re not missing another underlying problem), and even episodic syndromes that may be associated with migraine, such as stomach problems or sudden vertigo.
Now that you’re completely confused, you may be asking yourself – Who cares?! If I get a migraine, I take a pill! Why do I need to know all this?
There are some very important reasons why you should not settle for the “migraine” diagnosis, especially if you’re experiencing symptoms such as visual aura or weakness or vertigo or anything beyond just nausea, photophobia and phonophobia.
- A specific diagnosis shows that your doctor is knowledgeable. All right, I understand that many doctors don’t want to confuse their patients, and that a simple “migraine” diagnosis may be all that is needed. But if you ask, your doctor should be able to get more specific, and explain why she diagnosed you as she did.
- A specific diagnosis helps rule out other disorders and diseases. As I mentioned above, certain types of migraine may look like other disorders. Your doctor needs to do the proper tests and ask the proper questions, and that’s hard to do if he just says it’s “migraine”.
- A specific diagnosis can lead to better treatment. I understand that the treatment for many different types of migraine may be the same. However, a specific diagnosis can lead you to treatments that have been shown to be especially effective for that specific type.
- A specific diagnosis can help others. In today’s world, researchers are increasingly understanding the value of collecting data about migraine, whether by a clinical trial, an app, or a collection of information from doctors. Even when you leave a comment on a website or tell your story in a forum, it will help others far more if you can explain what kind of migraine you’ve been diagnosed with. What if we start hearing that many people with migraine with brainstem aura, for example, are being helped by a specific supplement or medication? We would never have known if these people had been lost in the ocean of “migraine patients”.
- A specific diagnosis can minimize confusion. How often do you hear that someone was diagnosed with ophthalmic migraine? complicated migraine? basilar migraine? or my favourite, cluster migraine? Well, they don’t exist – that is to say, they are not categories of migraine in the newest classification. And sometimes these names may have been used for very different types of migraine. Most of these names are out of date, and should be ditched. (A few are still out there just because of different points of view in the medical community – that’s a bit of a different issue.)
So – should we stop talking about “Migraine”?
I don’t really have a big issue with using the term “migraine” as an umbrella term, or if you’re not sure of your diagnosis yet, or if you’re talking to someone who doesn’t need the details.
As you probably know, I use the term here all the time.
But when you’ve taken the time to see a doctor and you’re investigating treatments, it’s time – personally – to see if you can get more specific information.
And your doctor may not be sure – and that’s all right. These things take time, and sometimes you have more than one type, or you need more time to really understand your symptoms. But an honest “this is what I think” or “I’m not 100% sure” is a lot better than “I don’t care” or “it doesn’t matter”. If you have a doctor with that attitude, it may be time to find a specialist.
If you’d like to start your research now, check out the official IHS Classification website. If you want the latest information, you can download the beta version of the newest classification system using the link in the right sidebar.