Are We Failing in the Fight Against Migraine?
Last year the well-known medical journal Headche published a study about migraine in the United States that was disturbing, to say the least. It seems that all the new awareness of migraine hasn’t had the impact that many hoped it would.
First of all, looking back over 30 years, the researchers found that the prevalence of migraine hasn’t changed much. About 13% or so of the population have migraine. In a group of 100, about 73 of those would be women, and 26 would be men.
Now, if you believe that migraine is a difficult-to-treat genetically based disease, you might say, “Sure, the number of people with migraine may not change much. But we’ve learned so much more about how to treat them – so these people now have better treatments, and so fewer and less severe attacks!”
Except, the data isn’t telling us that either.
Using the MIDAS test, which measures disability from migraine, the researchers found that the trend is generally toward more disability, not less. This chart gives you an idea how many people with migraine are suffering with moderate/severe disability.
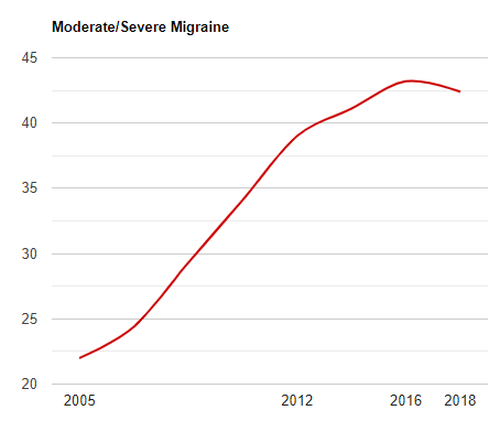
(Note – the study only had data for the years shown, so the graph is a smoothed-out estimate.)
It looks bad – and it is. However, we should note that there are some possible weaknesses in the study. For example, the estimates are only as good as the actual reports we get. Is it possible that more people are taking migraine seriously? More people are seeing their doctors?
Is the (slight) downward trend we see starting in 2018 a sign of things to come?
Maybe. But the results are still disturbing. The fact remains that the percent of migraine patients with significant disability almost doubled between 2005 and the most recent measurement!
Why aren’t we making more progress? Dr. Josh Turknett made some comments in December to consider. You can watch his video for yourself, but here are some points he made:
- Preventative medications often either don’t work, or only work temporarily.
- Abortive medications are also of limited use, often leading to – more abortive medications, and worse migraine disability.
He also implies (rightly, I think) that lifestyle changes are under-appreciated, to say the least. Many specialists may have better knowledge of migraine medications, and even better medications, but they’re still over-focused on prescribing medications and under-focused on things like diet.
By the way, I would recommend Dr. Turknett’s book to you – The Migraine Miracle. It’s a great place to start if you want to get beyond “the next pill” in your migraine treatment.
I would add some other thoughts about why we’re not doing as well as we could be in migraine treatment.
It could be argued that we have better, more targeted medications for migraine today. Although these medications seem to help some who have not been helped by other treatments, statistically speaking they also help those who might already be helped by another medication. In other words, saying that a certain medication may help 10% of migraine patients is not to say it will help another 10%. If that were the case, migraine would have been virtually eradicated by now.
The hype does not always match the reality. New medications come with new side effects, and they do not help everyone.
The hype can also take the focus away from lifestyle changes. There will always be a “new and better” migraine medication on the horizon. Don’t get me wrong – I think that research should continue, and that these medications may be helpful for certain people at certain times. But lifestyle is an incredibly powerful tool – to ignore it means that migraine will only get worse.
Having been involved in migraine research and advocacy for many years, I have seen many people who have found relief. The trend may be disturbing, but the trend does not have to be you. There is hope, and knowledge is an important step.
So even in the area of new medications and research of future medications, I do see a benefit. However, I agree that if we don’t take a serious look at the incredible healing power of lifestyle changes, the situation will not get better.