Yes, Children Get Cluster Headache Too
Although cluster headache usually starts in your 20s or 30s, children can, and do, get cluster too. Usually the symptoms start after the age of 10, but children with cluster have been reported as young as 6 years old.
 The fact that cluster headache is extremely rare in children is no comfort to children who get it and their families who are trying to help them. Although we’ve talked about cluster headache in children before, it’s time for an update.
The fact that cluster headache is extremely rare in children is no comfort to children who get it and their families who are trying to help them. Although we’ve talked about cluster headache in children before, it’s time for an update.
As with adult cluster, more males are diagnosed than females. However, a surprising number of girls get cluster as well.
But one of the biggest challenges is diagnosis. A study in 2009 of eleven children found that, on average, their symptoms began at the age of 8.5, but they went two years without a proper diagnosis.
Sadly, headaches in children are often considered to be caused by “stress” or “attitude”. However, a specialist who know what questions to ask can get to the truth a lot faster.
Another challenge is that cluster headache is not usually constant. Attacks typically last from 15 minutes to three hours. But they also go into remission. Headaches may occur once or several times a day for a while, and then disappear for months or years.
Symptoms in children tend to be similar to those in adults. That would include agitation and restless movement, one sided pain, congestion, and facial flushing and sweating. (For more detail, see Cluster Headache Symptoms)
Treatments for cluster are also similar to treatments in adults, partly because precious little study has been done specifically for children. One study found that oxygen, methysergide, verapamil, zolmitriptan and dihydroergotamine were particularly helpful for children, but that paracetamol/acetaminophen, ibuprofen and codeine with paracetamol/acetaminophen were not particularly helpful.
For more information:

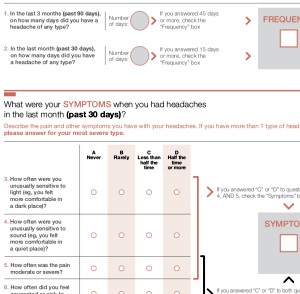 Enter ID-CM, otherwise known simply as Identify Chronic Migraine.
Enter ID-CM, otherwise known simply as Identify Chronic Migraine.
 You will still also have access to the extras like the Trigger Guides and Treatment Directory, and the Treatment Plan Checklist and 5 Mistakes Migraineurs Make booklets.
You will still also have access to the extras like the Trigger Guides and Treatment Directory, and the Treatment Plan Checklist and 5 Mistakes Migraineurs Make booklets. Do emotions play any part in migraine at all? Of course they do. But that doesn’t mean that they cause attacks, or that “controlling” them will make the pain go away (the insinuation being, of course, that the patient is 100% to blame for every attack, and that each attach is the patient’s choice!).
Do emotions play any part in migraine at all? Of course they do. But that doesn’t mean that they cause attacks, or that “controlling” them will make the pain go away (the insinuation being, of course, that the patient is 100% to blame for every attack, and that each attach is the patient’s choice!).