Migraine and Complications in Pregnancy
A recent press release from the American Academy of Neurology reports on a study of women with migraine, and what kinds of complications they may expect during pregnancy. Should potential mothers be concerned? And what can they do to prepare in advance?

This study took a look at about 30,000 pregnancies in about 19,000 women. Over 2000 of those women had been diagnosed with migraine. So how did their pregnancies differ from the rest?
Researchers did indeed conclude that women with migraine were more likely to have certain complications:
- Preterm Delivery – that is, delivery before 37 weeks.
- Gestational High Blood Pressure – hypertension during pregnancy
- Preeclampsia – another high blood pressure condition, often including signs of damage to the kidneys or liver.
The highest risk came with preeclampsia, a 40% higher risk, according to the study. This risk has been talked about for a long time – see Preeclampsia and Migraines.
It is, however, important to keep these numbers in perspective. Just how high is the risk?
From this study alone, this is what the risk of preeclampsia looks like:
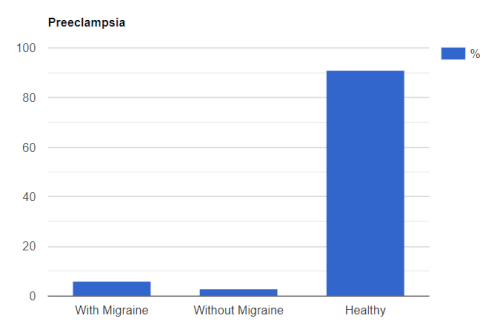
So note this. This “healthy” group includes people with migraine and without. So yes, far more people with migraine had preeclampsia than people without migraine who had preeclampsia. But your risk is still relatively low. And it’s a much better picture when it comes to hypertension and preterm delivery.
So what can you do? Actually, there are a number of things you can do to lower your risk even further, and keep your baby and yourself safe. For example:
- Lower your risk for high blood pressure in other ways. Talk to your doctor about the medications you’re taking. Aim for a healthy lifestyle overall, which will include exercise, plenty of water, a healthy diet, and avoiding alcohol, smoking, and certain drugs.
- Consider magnesium, which is a treatment for both migraine and preeclampsia. Read more at Preeclampsia, Migraine, and Magnesium
- Other supplements and medications may help, such as calcium and vitamin D. Talk to your doctor about these. (Note that for migraine you won’t want to take calcium at the same time of day as magnesium.)
- Talk to your doctor about your medical history.
- Talk to your doctor about any changed in headache or related symptoms. This is very important.
- Take a look at the Migraine During and After Pregnancy chart to know what you might expect during various stages.
- Don’t ignore migraine symptoms overall – talk to a specialist about the many, many treatments that are available.
- Check out The Myth-Busting Guide to Migraines and Pregnancy
Remember, although there seems to be some connection between migraine and some pregnancy risks, this study does not come anywhere close to telling us what the connection is. Yes, the researchers did adjust for some common risk factors to try to weed out weak connections. But we don’t know if there is some other common root cause, or if migraine symptoms may increase risk, or even if there is an unknown lifestyle connection.
The bottom line – it’s important to be aware of potential risks. But in most cases, these risks are small and manageable and no reason to avoid pregnancy.
This press release is only a preview of a report that will be given in April at the American Academy of Neurology’s 74th Annual Meeting. For more on the study, see Is migraine tied to complications in pregnancy?
