How To Really Rate Your Pain
“How bad is the pain, from 0 to 10?”
What does that question even mean? And if you’re not sure, how can you know it means the same thing to your doctor? Or your family?
 Sometimes this isn’t a big deal. When I was in the emergency room with a migraine attack, I was asked the question over and over. The doctor was most interested in the change, in the possible improvement. So if a “7” to me meant the same as an “8” to him, it didn’t matter too much, as long as I was relatively consistent. Then again, that’s not easy either, when you’re stupid with agonizing pain.
Sometimes this isn’t a big deal. When I was in the emergency room with a migraine attack, I was asked the question over and over. The doctor was most interested in the change, in the possible improvement. So if a “7” to me meant the same as an “8” to him, it didn’t matter too much, as long as I was relatively consistent. Then again, that’s not easy either, when you’re stupid with agonizing pain.
There are whole studies out there that try to find the best way to measure pain – which is incredibly hard with something so objective.
In fact, the type of pain, and other symptoms, can make a huge difference. For example, if I said,”I’m in so much pain, I can’t move”, what does that mean? If I had a severe laceration, I might still drive myself to the hospital. If I had comparable pain all over my body, I might be writhing in pain. With cluster headache, I might be pacing. If it was pain + nausea, even moderate pain could be incapacitating.
Ok, so here are some quick tips. Don’t make it too complicated, but do try to be as accurate and consistent as you can. Thinking about this before you’re in severe pain could be a big help.
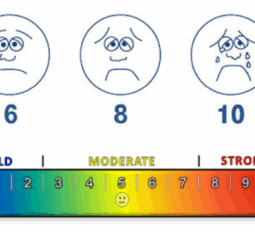
- Pick a pain scale and stick with it. I’ll link to some ideas below. There are pain scales for certain diseases. There are also pain scales that work better with children. Or, you can have a child draw their pain. Whatever you choose, understanding it and sticking with it will help you measure changes in your condition over time.
- Make sure you and your doctor speak the same language. I don’t mean English or Spanish, but make sure you both understand what’s expected from the pain scale. In a recent article, Beth Skwarecki discovered that a simple question or two can clarify a whole lot. In my case, I have always thought of a ten as a theoretical maximum before passing out. But that’s not what many doctors think. This could be hard in the emergency room, but for a doctor you regularly see, it’s worth getting on the same page.
- Become increasingly aware of other symptoms. And with migraine, there can be a wide variety. As in the nausea example above, nausea can totally incapacitate you – as can dizziness, muscle weakness, and so on. The disability of many migraine attacks is not just from the pain. We often are not aware of other symptoms because we focus on the pain. If your symptoms are fairly consistent, you can even explain the “type” of headache you have (I used to use 6 classifications of my own, based on symptoms I experienced).
- If you’re aware of those three things, you’ll be way ahead of most people when it comes to explaining your pain.
Now, Beth’s article above leads to some great links, but this is one you really should take a few minutes to read: 15 Pain Scales (And How To Find The Best Pain Scale For You)
These can give you some very useful ideas. Don’t miss #2 (common) #11 and #14. Similar to #11 is the Stanford PainScale, which would be a great thing to print out or put on your phone and show your doctor (that might even work in emergency – keep it with any papers you might bring along).
Now you’re armed and ready to really explain your pain – hopefully that will lead to better treatment ASAP!
