Let’s talk about “Brain Organoids”.
Migraine research, and research on the brain and nervous system, has come a long way in the past 30 years. But researchers are only partially aware of how far we have to go.
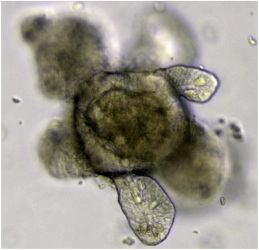
(photo courtesy Meritxell Huch)
Why? Because the human brain is incredibly complex. Few people realize just how little we know about how it works – and, in fact, how the human body as a whole works.
Here’s one of the big challenges when it comes to migraine research. When you’re investigating a new medication, traditionally you’ll have animal trials. Normally you will have safeguards for the animals too, but you do this so that the higher risk goes to the animal and not to the human.
But ethical questions aside, the fact is that the brain of a rodent is incredibly different from the brain of a human being (which is perhaps why Pinky and the Brain haven’t taken over the world). And so medications that may show some promise in the animal turn out to be useless in the human. A waste of time and money.
Brains of deceased humans have also been studied for migraine research – but as you may guess, there are severe limitations to that as well.
So, what if we could test a human brain – or at least some “living” human brain tissue – or any part of the body, for that matter, without actually hurting a human? Enter organoids.
Organoids are tiny 3D bits of human organs grown in the lab. And you have already guessed what brain organoids are. Another step is to take different organoids and put them in a system, so that you can test human-like organ systems. This is done using – no kidding – “assembloids”. But as you can imagine, this is way beyond putting together an Ikea shelf.
These systems can be put together to model certain diseases, such as Parkinson’s or Alzheimer’s. We can learn more about how these diseases work, and even test out treatments.
This is a very promising field of study, but there are two big hurdles. First, the challenges/limitations of the process as it exists today. Second, ethical/wider dangers concerns.
This amazing technology is not without its limitations. For example, scientific study requires a limitation and understanding of variables. Today, there is a variety of methods in the organoid world, and even if you standardize the methods, it’s very hard to get things exactly the same every time. Scientists need to find methods that will limit the variables.
Also, it’s a challenge to create a system complex enough to truly help us understand the migraine chain reaction. We will always be getting a partial view of what’s going on in the human body.
There are a host of ethical concerns as well, including concerns about the dangers of some types of organoid research in particular. For example:
- Does the original tissue come from an ethical source? Was anyone harmed in the process?
- What are the limitations to combining human and non-human tissue? Both animal rights and human rights activists will have problems here. This is called chimera research – when tissue/DNA from more than one species are combined. And we’re especially talking about human tissue. This type of experimentation could have series consequences for the futures of more than one species if it goes the wrong way.
- How complex are these systems going to be? What if we can create a self-aware human being, for example?
- What about genetic manipulation? What if those genetic changes affect the human species in general?
And remember, although we’re very thankful for ethical migraine research, there are many doing experimentation around the world for reasons which may include the intent to harm, not to help.
Most of these hurdles can probably be overcome in theory. Excuse the cliché, but I think we all hope that this powerful tool will be used for good and not evil. It has great potential when it comes to migraine research, so we look forward to seeing what is to come in the years ahead.
To read more, check out Human Brain Organoids in the Preclinical Phase of Drug Development for Migraine, and Ethical issues in human organoid and gastruloid research. Also helpful: Human Brain Organoids in Migraine Research: Pathogenesis and Drug Development