Warning Flag: Do you have non-headache pain?
It’s actually very common for migraine patients to suffer from non-headche pain – that is, back pain or leg pain or face pain or neck pain – and so on. But could this kind of pain be warning us that things are going to get worse?
Dr. Ann Scher and her team studied the symptoms of nearly 13,000 migraine patients to see how non-headache pain – that is, non-cephalic pain, related to the progression of migraine disease. The researchers then compared non-cephalic pain with migraine frequency.
For example, if you have episodic migraine (fewer than 15 attacks per month), chronic migraine (more than 15 attacks but not daily) or daily chronic migraine, how many other “pains” do you have? That is, how many other locations are manifesting pain? This chart shows the differences:
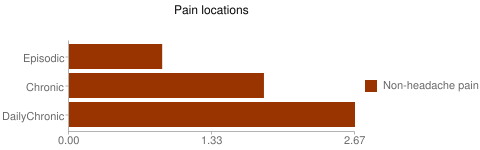 So the more chronic the disease, the more pain locations (see study at Pain Comorbidities of Episodic and Chronic Migraine).
So the more chronic the disease, the more pain locations (see study at Pain Comorbidities of Episodic and Chronic Migraine).
In fact, nearly half of those with chronic daily migraine had severe pain in another location, whereas less than 20% with episodic migraine did.
But what if you have episodic or chronic (non-daily) migraine? Do these other pains increase your chances to progress to a worse version of the disease?
The answer seems to be yes.
 For each non-cephalic pain location, patients with episodic migraine were 30% more likely to progress to chronic. For patients who were already chronic, each pain location increased their odds by 6% to stay chronic. Read more at Noncephalic pain sites shed light on progression from episodic to chronic migraine.
For each non-cephalic pain location, patients with episodic migraine were 30% more likely to progress to chronic. For patients who were already chronic, each pain location increased their odds by 6% to stay chronic. Read more at Noncephalic pain sites shed light on progression from episodic to chronic migraine.
One theory is that there is an underlying genetic condition that is triggering both pains. It’s certainly not unusual for migraine patients to be more sensitive to pain. There also could be something else that is worsening pain symptoms and worsening the migraine disease, such as the type of medication a patient is taking.
This is another study which helps us understand the progression of the disease. It is, at the very least, another warning flag for patients and their doctors. If there is pain in more than one location, the migraine attack should be taken all the more seriously before they have a chance to get worse.
As a side note, although this study was supported by Allergan, Dr. Ann Scher is also supported by the Migraine Research Foundation. To support further research, click here if you’re in the United States, here if you’re elsewhere.

14 September 2015 @ 4:15 pm
Never really thought of migraine as a progressive condition – useful to know that people are starting to think about it that way. I am more sensitive to pain and always have been even as a child before migraines developed. Sometimes everything hurts! It would be nice to have a day when I do not have some part of my body hurting.
14 September 2015 @ 5:53 pm
I have found treating a systemic infection, likely chronic Lyme disease years after contracting it, also helped my headaches. I suggest various infections, including EBV, could cause widespread pain over the years.