Very Different “CGRP Drugs”
With our current obsession with the four magic letters, “CGRP”, and the CGRP related drugs that are now hitting the market, many people have not realized that there are two very different types of CGRP drugs out there. So here’s a quick description to get you up to speed.
What is “CGRP”?
CGRP (calcitonin gene-related peptide) refers to a peptide, a type of amino acid, that is naturally in your body. A lot of study is currently being done regarding the connection between CGRP and pain. It does seem to play a key role in the way your body responds to pain, inflammation, and migraine in particular. It may be that problems with CGRP function may cause you to become overly “sensitive”, leading to chronic migraine and other chronic pain conditions. However, we still have a lot to learn about how it works.
Blocking CGRP?
So if we somehow block CGRP, could we lessen the symptoms of migraine, or even stop migraine in its tracks? Well, that does seem to be the case with some people. We could either do this in a preventative way – that is, take a medication regularly to keep CGRP under control. Or perhaps we could use it to stop a migraine attack that has already started – that is, use it as an abortive. But how do we actually lower levels of CGRP?
CGRP Inhibitor
What if we could target CGRP itself? That’s the goal of the new preventative drugs that are hitting the market now. They’re called CGRP inhibiting monoclonal antibodies (mAbs). These include erenumab (Aimovig), galcanezumab (Emgality), fremanezumab (Ajovy), and eptinezumab. These are taken by injection either monthly or quarterly in order to lessen migraine attacks and symptoms. You’ll notice that these drugs use mAb in their names.
CGRP Receptor Antagonists
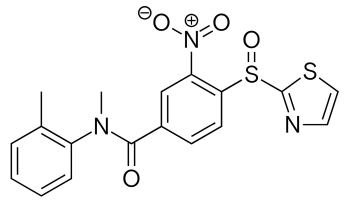
“Inhibitor” and “Antagonist” have a similar meaning, but you’ll notice that in this case the target is slightly different. Instead of targeting CGRP itself, we go for the CGRP receptor. These drugs work very quickly, but they’re not getting to the market as fast because they’re being carefully studied to make sure adverse reactions are minimal.
However, because they are “fast” they should make great abortives – something to take when the migraine attacks hit. These are the “gepant” drugs – such as ubrogepant and rimegepant. Also called a receptor “blocker”, the mechanism is complicated but you can think of it as another way to keep CGRP from functioning, hopefully lessening migraine symptoms during an attack.
And then…
There are several other types of migraine drugs on the way, each with a different way of attacking migraine. These include 5-HT1F agonists, and anti-PAC 1 drugs. We’ll try to talk more about these in the future. But the idea is to stop the migraine chain-reaction so that symptoms are lessened or stopped. Ideally, the closer we get to the “source” of migraine, the more we’ll be able to stop it altogether.